How Elimination Diets Reduce Dairy-Related Inflammation
Eliminate dairy for 4-8 weeks and reintroduce it to identify sensitivities, lower inflammatory markers, and personalize your diet.

Elimination diets help identify and manage dairy-related inflammation by temporarily removing dairy and then reintroducing it to observe symptoms. For some, dairy can cause inflammation due to lactose intolerance, protein sensitivities, or allergies. Symptoms often stem from undigested lactose, immune responses to milk proteins, or saturated fats in dairy triggering inflammatory markers.
Key points:
- Lactose intolerance: Causes bloating and discomfort when lactose ferments in the gut.
- Milk protein sensitivities: Can trigger immune responses and inflammation.
- Saturated fats: Found in dairy, may activate inflammation pathways.
- Elimination diets: Remove dairy for 4–8 weeks, then reintroduce it gradually to pinpoint triggers.
- Fermented vs. non-fermented dairy: Fermented options like yogurt may reduce inflammation, while non-fermented dairy can sometimes increase it.
Research shows this approach is effective for conditions like eosinophilic esophagitis and may help manage symptoms in other inflammatory conditions. Tracking symptoms and consulting with a dietitian ensures better results and balanced nutrition.
We Need to Talk About Dairy and Lipedema (The Best and Worst Choices)
What Are Elimination Diets and How Do They Work?
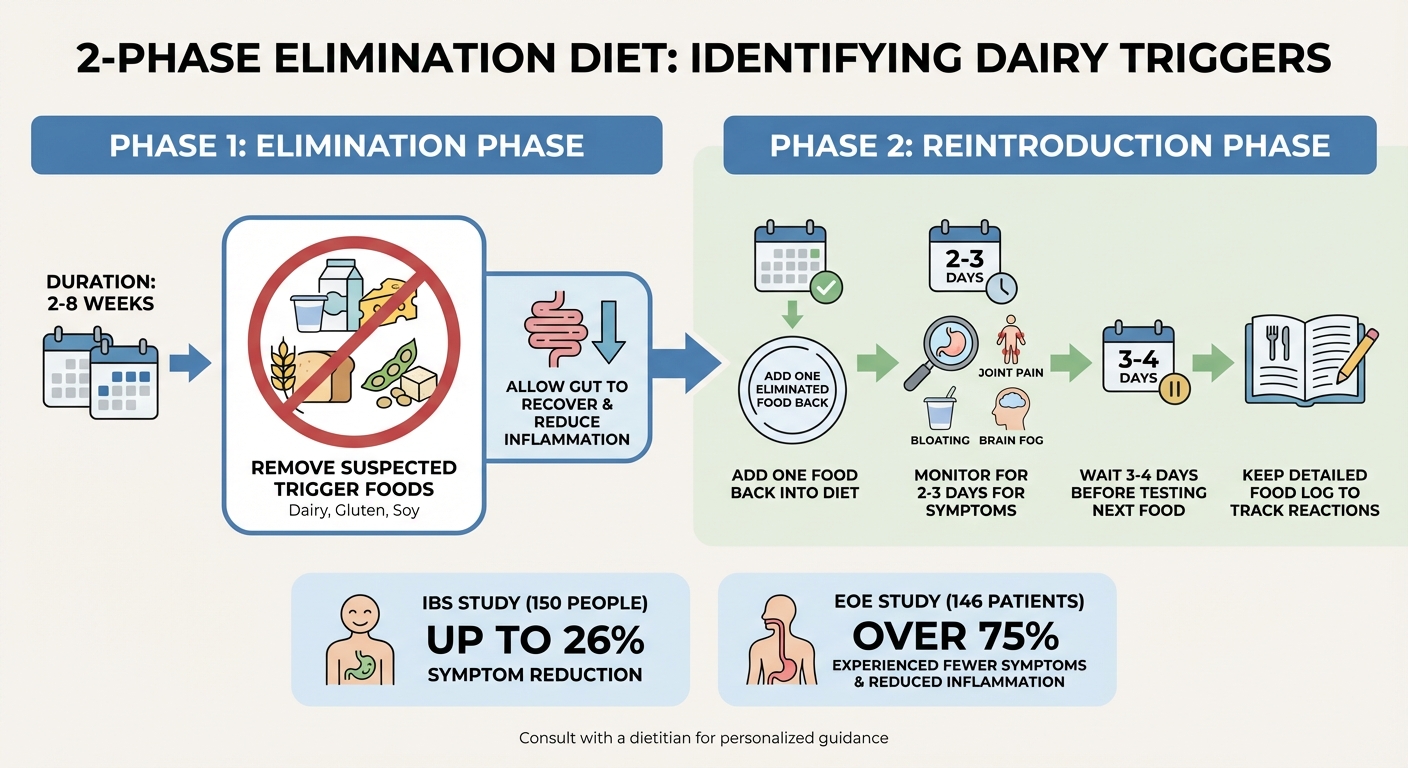
How Elimination Diets Work: 2-Phase Process for Identifying Dairy Triggers
Elimination diets involve temporarily removing specific foods from your meals to identify potential allergens or sensitivities that might be causing health issues. The process is broken down into two key phases, each designed to help pinpoint which foods are problematic.
The first step, called the elimination phase, lasts 2–8 weeks. During this time, you cut out suspected trigger foods like dairy, gluten, or soy. This break allows your gut to recover and reduces inflammation caused by these foods. For example, focusing solely on eliminating dairy - especially animal milk - has been shown to help achieve remission in conditions like eosinophilic esophagitis.
Next comes the reintroduction phase, where you gradually add the eliminated foods back into your diet, one at a time. Over 2–3 days, you monitor for symptoms like bloating, joint pain, or brain fog, and then wait 3–4 days before testing another food to catch any delayed reactions. Keeping a detailed food log during this stage can help you connect specific foods to symptoms. This careful, step-by-step process makes it easier to identify which foods are causing issues, including whether dairy is a culprit.
Research supports the effectiveness of elimination diets. For instance, a 2004 study involving 150 people with IBS found that those who followed an elimination diet reduced their symptoms by up to 26%. Similarly, a 2005 study on 146 patients with eosinophilic esophagitis revealed that over 75% experienced fewer symptoms and reduced inflammation after adopting an elimination diet.
How Dairy Triggers Inflammation
Now that we’ve covered the diet process, let’s dive into why dairy can sometimes cause inflammation.
Dairy triggers inflammation through different biological pathways, depending on how your body reacts to its components. One common issue is lactose intolerance, which happens when your body doesn’t produce enough lactase - the enzyme needed to break down lactose, the sugar in milk. When lactose isn’t digested, it ferments in the colon, leading to gas, bloating, and other digestive discomforts.
Another factor is protein sensitivity. Milk proteins like casein and whey can sometimes pass undigested into the intestines, triggering a delayed immune response. These proteins may activate immune cells like Th1, Th2, or Th17, which release cytokines that contribute to inflammation by stimulating neutrophils or epithelial cells.
Additionally, palmitic acid in dairy can activate TLR4 receptors on macrophages, leading to the production of inflammatory cytokines.
To measure the impact of dairy on inflammation, healthcare providers often track specific markers in your blood, such as C-reactive protein (CRP), Interleukin-6 (IL-6), and Tumor Necrosis Factor-alpha (TNF-α). For instance, CRP levels can spike dramatically during an inflammatory response, jumping from a baseline of ≤1 mg/L to over 100 mg/L. These biomarkers provide a clear, measurable way to assess whether dairy is contributing to inflammation in your body.
Scientific Evidence: Dairy Elimination and Inflammation Reduction
Clinical trials have explored how removing dairy from the diet impacts inflammation, revealing varying results based on individual factors like allergies or sensitivities. For some, dairy elimination has shown clear benefits, while for others, it may not be as impactful.
Key Research Findings
One of the strongest cases for dairy elimination comes from studies on Eosinophilic Esophagitis (EoE), a chronic inflammatory condition of the esophagus where dairy is a major trigger. In May 2023, a multicenter trial involving 129 adults with active EoE compared two dietary approaches. One group eliminated only dairy for six weeks, while the other followed a six-food elimination diet. Interestingly, cutting out dairy alone was just as effective as eliminating all six foods in reducing esophageal inflammation.
A 2023 meta-analysis of 34 studies with 1,762 participants found that a one-food elimination diet focused on dairy achieved a 51.4% histologic remission rate in EoE patients. Pediatric patients responded even better, with a 55.3% remission rate, compared to 34% in adults. Supporting this, an April 2016 study by Elizabeth A. Erwin, published in the Journal of Allergy and Clinical Immunology, showed that 62% of pediatric patients (13 out of 21) experienced a significant drop in esophageal eosinophil counts after 6–8 weeks of eliminating cow’s milk.
| Dietary Regimen | Histologic Remission Rate | Clinical Response Rate |
|---|---|---|
| 1-Food Elimination (Dairy) | 51.4% | 87.1% |
| 4-Food Elimination | 49.4% | 74.1% |
| 6-Food Elimination | 61.3% | 92.8% |
For individuals without a dairy allergy, the findings are more nuanced. A systematic review of 17 trials revealed that in overweight and obese populations, four studies actually observed a reduction in CRP levels (a marker of inflammation) with dairy consumption. For example, an 8-week study involving 75 overweight adults found that those consuming probiotic yogurt as part of a low-calorie diet saw significant decreases in inflammatory markers like hs-CRP, IL-17, and TNF-α compared to control groups.
"A 1-food elimination diet removing animal milk has proved comparable to the 6-FED in achieving histological remission in patients with eosinophilic esophagitis." - Jordan C. Malone, University of Texas Medical Branch
Impact on Chronic Inflammatory Conditions
Dairy elimination may also benefit those with other chronic inflammatory conditions. For example, in rheumatoid arthritis (RA), dairy proteins are thought to contribute to inflammation through a process known as "leaky gut." This occurs when the intestinal lining becomes more permeable, allowing toxins and undigested food particles to enter the bloodstream and trigger widespread inflammation.
Diana Girnita, MD, PhD, a rheumatologist, explains:
"Intestinal permeability ('leaky gut') allows toxins, bacteria, and undigested food particles to enter the bloodstream, triggering widespread inflammation."
Patients with RA are often advised to eliminate dairy for a four-week trial to assess improvements in joint pain and swelling. Notably, about 20-30% of individuals with RA also have sensitivities to gluten, which can similarly increase intestinal permeability.
The research underscores that dairy's inflammatory effects depend largely on individual sensitivity. As one review put it, dairy can exhibit "anti-inflammatory activity in subjects with metabolic disorders and pro-inflammatory activity in subjects allergic to bovine milk". This is why elimination diets, followed by careful reintroduction of foods, are essential for determining whether dairy is inflammatory for you.
How Eliminating Dairy Reduces Inflammation
Cutting dairy from your diet can directly lower inflammation by removing certain components that trigger inflammatory processes.
For instance, avoiding dairy eliminates palmitic acid, a saturated fat that promotes the production of pro-inflammatory cytokines. This fat, commonly found in dairy, contributes to the formation of "crown-like structures" - clusters of inflammatory cells around stressed fat cells. Over time, these structures raise inflammatory markers like hs-CRP and IL-6. While healthy individuals generally maintain CRP levels at or below 1 mg/L, chronic exposure to saturated fats can disrupt this balance.
"Extracellular SFAs, including palmitic acid (16:0), which is the most abundant fatty acid in milk, can directly activate TLR4 signaling by macrophages... this activation can trigger production of proinflammatory cytokines."
- Julie M. Hess, National Dairy Council
Reducing or eliminating high-fat dairy products such as cheese, butter, and cream can significantly lower your intake of these saturated fats. This shift may be particularly beneficial for individuals dealing with metabolic conditions or dairy sensitivities, as it helps reduce levels of pro-inflammatory biomarkers. However, it's worth noting that not everyone responds to dietary changes in the same way. Interestingly, the effects of eliminating high-fat dairy differ from the potential benefits linked to fermented dairy products.
Fermented vs. Non-Fermented Dairy
Dairy products don’t all have the same effect on inflammation. Research from 52 clinical trials highlights a clear distinction: fermented dairy products like yogurt and kefir consistently reduce inflammatory markers, while non-fermented options such as milk, butter, and cream tend to show neutral or even pro-inflammatory effects. The anti-inflammatory properties of fermented dairy are largely due to their probiotic content, which supports a healthier gut microbiome.
"Yogurt is associated with decreased inflammation, decreased insulin resistance and it may prevent type 2 diabetes."
- Frank Hu, MD, PhD, Harvard T. H. Chan School of Public Health
| Dairy Type | Effect on Inflammation | Key Mechanism |
|---|---|---|
| Fermented (yogurt, kefir) | Anti-inflammatory | Probiotics support gut health; lower IL-6 & hs-CRP |
| Non-Fermented (milk, butter, cream) | Neutral to pro-inflammatory | High SFA content activates TLR4 pathway |
Using Elimination Diets as a Long-Term Strategy
Elimination diets are more than just short-term fixes - they can help pinpoint specific food triggers while supporting a balanced and sustainable way of eating.
Phased Elimination and Reintroduction
The process starts with a strict elimination phase that typically lasts 4–8 weeks. During this time, all dairy is removed from your diet to allow the gut to heal and reduce inflammation. Sticking to the plan is critical - any slip-ups can reignite inflammatory responses.
Afterward comes the reintroduction phase, which requires just as much care. Introduce one dairy product at a time over a 2–3 day period. This gradual approach helps identify your tolerance levels while minimizing potential reactions. Keeping a detailed food diary during both phases is key. Record not just digestive symptoms but also changes in mood, energy levels, headaches, sleep quality, and any physical discomfort. These notes can uncover patterns that might otherwise go unnoticed.
It's also important to work with a Registered Dietitian Nutritionist (RDN) to avoid nutritional gaps, especially in nutrients like calcium and vitamin D that are plentiful in dairy. The goal here isn’t to eliminate dairy forever - it’s to understand how much your body can handle. For instance, many people find they can consume up to 12 grams of lactose (about one cup of milk) without triggering inflammation. For those who can tolerate small amounts of dairy, additional strategies can help expand dietary options.
Enzyme Support for Dairy Sensitivity
Enzyme supplements can be a helpful addition for those managing dairy sensitivities. If dairy triggers symptoms but you’d rather not cut it out entirely, these supplements can bridge the gap. They work by breaking down dairy components that the body struggles to process. For example, lactase enzymes convert lactose into glucose and galactose, preventing bacterial fermentation in the colon that often causes bloating, gas, and inflammation.
A product like milktab offers a comprehensive solution with its triple-enzyme formula. Each pill contains 27,000 FCC units of lactase, 22,000 FCC units of protease (to break down dairy proteins), and 1,000 FCC units of lipase (to digest dairy fats). This formulation tackles multiple triggers in one dose. It’s vegan, non-GMO, FODMAP-free, and third-party tested, with a recommended maximum of two pills per day.
Enzyme supplements are especially useful during the reintroduction phase, allowing you to test dairy products without discomfort. Over time, they can provide more dietary flexibility and ensure you’re still getting essential nutrients while managing symptoms effectively.
Conclusion
Elimination diets can help uncover and manage dairy-related inflammation. By removing dairy for 4–8 weeks and gradually reintroducing it, you can gain important insights into your body's specific triggers and tolerance levels. As Sharon Jaeger, a Registered Dietitian at Cleveland Clinic, explains:
Elimination diets are the gold standard for figuring out which food don't agree with you.
There's no universal approach that works for everyone. While some individuals may need to avoid dairy completely, others might find they can handle fermented products like yogurt or small amounts of specific dairy items. With studies indicating that up to 20% of people globally experience food intolerances, tailoring your approach is key for long-term success. Personalized strategies, including enzyme supplementation, can also be part of this process.
It's important to consult with a dietitian to ensure you maintain essential nutrients in your diet. The aim isn’t to restrict permanently but to develop a sustainable eating plan that aligns with your body's unique needs.
For those who can tolerate some dairy, enzyme supplements can provide flexibility. Options like milktab, featuring a triple-enzyme formula with 27,000 FCC units of lactase, 22,000 FCC units of protease, and 1,000 FCC units of lipase, allow for dietary variety while helping reduce inflammation. By understanding how your body reacts, you can make informed choices that support both digestive health and overall well-being.
FAQs
How can I tell if dairy is causing inflammation in my body?
If you think dairy might be causing inflammation, start by observing how your body feels after you consume it. Some common signs of sensitivity include bloating, gas, diarrhea, or even joint pain. Since everyone reacts differently, an elimination diet can be a helpful way to figure out if dairy is the culprit. This involves cutting out all dairy products for a few weeks and then gradually reintroducing them while keeping an eye on any changes in your symptoms.
The research on dairy and inflammation is mixed - some studies suggest it could promote inflammation, while others indicate it might have anti-inflammatory properties. Because of this, your personal experience matters most. Consulting with a healthcare provider or dietitian can provide guidance, ensuring you approach this process safely and still get the nutrients your body needs.
How do fermented and non-fermented dairy differ when it comes to inflammation?
Fermented dairy products like yogurt and kefir tend to be linked with a lower inflammatory response compared to their non-fermented counterparts. Studies suggest that these options may affect gene expression in ways that decrease pro-inflammatory activity.
The key difference lies in the probiotics and bioactive compounds found in fermented dairy. These components can help support gut health, which may play a role in reducing inflammation. If you're navigating an elimination diet and considering dairy, fermented options could be worth trying - depending on your personal tolerance.
Can lactase enzyme supplements help me digest dairy if I want to reintroduce it into my diet?
Yes, taking lactase enzyme supplements can make it easier to digest dairy, particularly if you're lactose intolerant. These supplements help by breaking down lactose - the sugar found in dairy - making it less likely to cause issues like bloating, gas, or stomach discomfort.
That said, if you're planning to add dairy back into your diet, it's best to do it slowly and carefully. Monitor how your body reacts, and if you're uncertain about the right steps for you, it’s a good idea to check in with a healthcare professional.



