Reintroducing Dairy After an Elimination Diet
Learn how to safely reintroduce dairy after an elimination diet to identify your lactose tolerance and manage symptoms effectively.

Reintroducing dairy after an elimination diet can help you determine if your body tolerates lactose or dairy products, and to what extent. This process involves removing dairy for a few weeks, then gradually reintroducing it while monitoring your body's reactions. Here's a quick overview:
- Why Reintroduce Dairy? To identify lactose intolerance or sensitivity and establish your personal tolerance level.
- Steps to Follow:
- Start with low-lactose options like butter, ghee, or aged cheeses.
- Gradually increase portions over several days.
- Use a symptom log to track reactions like bloating, cramping, or skin changes.
- Follow the "milk ladder" to reintroduce dairy in stages, starting with baked goods and ending with fresh milk.
- Key Tools: Keep a symptom journal and consider lactase enzyme supplements (e.g., milktab) to ease digestion during the process.
- When to Stop: Severe symptoms like vomiting, swelling, or difficulty breathing require medical attention. Consult a doctor if symptoms persist or worsen.
This method helps you safely reintroduce dairy while understanding your body's limits, ensuring you can make informed dietary choices.
Elimination Diet: The BEST At-Home Test for Food Sensitivities | Inflammation | Autoimmunity
What Is an Elimination Diet?
An elimination diet is a method used to pinpoint food intolerances. Ryan Raman, MS, RD, explains:
"An elimination diet involves removing foods from your diet you suspect your body can't tolerate well. The foods are later reintroduced, one at a time, while you look for symptoms that show a reaction."
This approach is particularly helpful for identifying issues like lactose intolerance.
The process typically spans 5–6 weeks and is divided into two main phases. The elimination phase, lasting 2–3 weeks, involves cutting out foods that might be causing symptoms. Common culprits include dairy, wheat, gluten, eggs, soy, nuts, corn, citrus fruits, nightshade vegetables, pork, and seafood.
Next comes the reintroduction phase, where you reintroduce one food at a time over 2–3 days while monitoring your body's response. If symptoms return after eating a particular food, it’s likely a trigger and should be avoided.
This method is especially relevant since up to 20% of people worldwide may have some form of food intolerance. For lactose intolerance, the numbers are striking - around 70% of adults globally have reduced lactase enzyme levels. This makes elimination diets a practical starting point for diagnosis.
By following this structured approach, you can establish a reliable baseline for safely testing foods like dairy.
Why Use an Elimination Diet
Elimination diets are a practical way to identify food intolerances, especially when it comes to reintroducing dairy. By allowing your body to reset, this method provides clarity on which foods trigger symptoms. For example, removing potential allergens like dairy can improve symptoms before you begin testing your tolerance.
Compared to other diagnostic methods, elimination diets offer some key advantages. Research highlights their effectiveness when combined with oral food challenges:
"Employing an elimination diet with oral food challenges in patients with allergies and intolerances can be a cost-effective and noninvasive method of identifying trigger foods."
This approach works by first removing lactose from your diet and observing any symptom relief. Then, reintroducing lactose helps confirm whether it’s the cause of your discomfort. Unlike medical tests like hydrogen breath tests or lactose tolerance tests, which may not be accessible to everyone, elimination diets can be done at home and provide practical insights.
Another benefit is that they show how your body reacts to foods in real-life settings. Laboratory tests might measure biological markers, but elimination diets reveal how specific foods impact your daily comfort and well-being.
Additionally, this process can help you understand the severity of your intolerance. Some people find they can handle small amounts of dairy, even if larger portions cause issues. Knowing this can be key to creating a sustainable, long-term eating plan.
When to Start Adding Dairy Back
Once you've established a symptom-free baseline, timing is everything when reintroducing dairy. Experts recommend waiting a few days without symptoms before starting. This ensures that any reactions during reintroduction are directly linked to dairy.
The length of the elimination phase depends on your sensitivity. For non-IgE mediated cow's milk allergies, 2–4 weeks of elimination is typical before reintroduction. IgE-mediated allergies, however, may require only 1–2 weeks.
It’s critical to seek professional advice before reintroducing dairy. The North West Allergy Network stresses:
"Cow's milk reintroduction should only to be performed after obtaining advice from your doctor or dietitian."
This guidance is especially vital if you’re eliminating multiple food groups or suspect a true milk allergy rather than lactose intolerance. A healthcare professional can ensure you maintain proper nutrition during the elimination phase and guide you through the reintroduction process.
If symptoms persist after 2–3 weeks of removing dairy, consult your doctor. This could mean dairy isn’t the issue, or that there’s another underlying condition requiring further investigation.
How to Prepare for Dairy Reintroduction
Approaching dairy reintroduction with a clear plan helps you pinpoint any reactions without confusing them with stress or other dietary changes.
Keep a Symptom Log
A symptom log can be an incredibly useful tool when reintroducing dairy. It helps you spot patterns, identify triggers, and provides valuable information if you need to consult with a healthcare professional.
Record the following details in your log:
- Time: When you consumed dairy.
- Type and amount: The specific dairy product and quantity.
- Symptoms: Note any digestive issues like bloating, gas, cramping, or diarrhea, as well as non-digestive reactions such as skin changes, headaches, or mood shifts.
- Symptom details: Include onset time, intensity (rate it on a scale of 1–10), and how long the symptoms lasted.
It’s also helpful to track your baseline symptoms during the elimination phase. This gives you a point of comparison, so you can tell whether any changes are due to dairy or just regular fluctuations.
To stay consistent, use a method that works best for you - whether it’s a smartphone app or a simple notebook. Also, consider adding context like sleep quality and stress levels to better understand how your body responds to dairy.
Set Up a Stable Testing Environment
Once your symptom log is ready, create a calm and consistent environment to minimize external factors that could affect digestion. Stress and major life changes can make it harder to determine if symptoms are related to dairy or other influences.
Timing matters. Avoid starting the reintroduction process during high-stress periods or significant life events, like moving, traveling, or handling tight deadlines. These situations naturally impact digestion and could skew your results.
Choose a relaxed time when your digestion feels stable. Testing in the morning or at lunchtime works well because you’ll have plenty of daylight hours to observe any reactions. Stick to your elimination diet for all other meals to isolate the effects of dairy.
Set up an ideal eating environment: sit at a table, chew your food thoroughly, and take a few deep breaths before eating. These small steps can aid digestion and help you monitor your body’s response more accurately.
For the best results, plan your reintroduction at home during a quiet period. Avoid scheduling it near major events or travel, so you have access to familiar surroundings and can focus on tracking symptoms without added stress.
Step-by-Step Dairy Reintroduction Process
Reintroducing dairy into your diet requires a careful approach to identify your tolerance level while keeping digestive discomfort to a minimum. Here's a guide to help you navigate this process smoothly.
Start with Low-Lactose Options
Low-lactose dairy products are a gentle way to ease back into consuming dairy. Butter and ghee are excellent starting points, as they contain only about 0.1 grams of lactose per 3.5 ounces, compared to the 12–13 grams found in a cup of milk. Begin with a teaspoon of butter mixed into your food or a small dollop of ghee on cooked vegetables. Ghee, in particular, is often easier to digest since it has most milk proteins removed during clarification.
Once butter or ghee is well-tolerated, try aged, hard cheeses like cheddar, Parmesan, or Swiss. These cheeses typically have just 0.3–1 gram of lactose per ounce. Start with a 1-ounce serving and see how your body responds. The aging process naturally reduces lactose content, making these cheeses a safer choice than softer, fresher varieties.
Next, consider introducing full-fat, plain Greek yogurt. It contains about 2–4 grams of lactose per 4–6 ounce serving. The live cultures in yogurt help break down lactose, and studies show it can reduce the amount of undigested lactose in the digestive tract by about 60% for those with lactose intolerance.
Gradually Increase Portions
When introducing a new dairy product, take it slow. Stick to one-quarter serving sizes for 2–3 days, then gradually increase the portion. Choose breakfast or lunch for testing new foods, so you have plenty of time during the day to monitor for any symptoms.
Pair dairy with other foods to slow digestion and reduce the risk of discomfort. For example, enjoy cheese with crackers, mix yogurt with granola, or add a splash of milk to cereal instead of drinking it plain. If symptoms occur, step back to the last product you tolerated and wait until symptoms resolve before trying again.
If this gradual method feels too challenging, consider using the milk ladder approach.
Follow the Milk Ladder Approach
The milk ladder is a structured way to reintroduce dairy, starting with highly processed products where milk proteins are altered by cooking. This makes them less likely to cause reactions. Each step typically lasts about seven days before progressing:
- Step 1: Begin with baked goods containing milk, like malted milk biscuits or shortcake. High heat breaks down many of the proteins that can trigger reactions.
- Step 2: Move to baked items such as plain cakes, muffins, or scones, where milk is cooked but less extensively processed than in Step 1.
- Step 3: Try foods cooked for shorter periods, like scotch pancakes or snacks with cheese powder flavorings.
- Step 4: Introduce minimally cooked dairy, such as cream cheese on toast, macaroni and cheese, or pizza.
- Step 5: Test less processed products like yogurt, soft cheese, and butter - items that undergo fermentation or minimal processing.
- Step 6: Finally, reintroduce fresh milk. To make the transition easier, consider mixing it with milk alternatives.
Research supports the effectiveness of this gradual progression. Studies show that about 80% of children with milk allergies outgrow them by ages three to five. Additionally, among individuals with confirmed dairy issues, 57% develop tolerance within a year when following structured reintroduction plans.
How to Track Symptoms and Know When to Stop
Once you’ve started keeping a symptom log, the next step is understanding which reactions signal a need for caution. It’s important to carefully monitor how your body responds to dairy, as symptoms can show up right away or take as long as two days to appear. This tracking helps you determine your personal tolerance levels and recognize when it’s time to seek medical advice.
Symptoms to Look Out For
Mild symptoms might include bloating, gas, stomach gurgling, or mild abdominal discomfort. These are fairly common during the initial stages of reintroducing dairy and often indicate your digestive system is adjusting to lactose. These symptoms usually appear within 30 minutes to 2 hours of eating dairy but can sometimes take up to a day or two to show up.
Severe symptoms, on the other hand, demand more urgent attention. These include intense abdominal pain, cramping, nausea, vomiting, and diarrhea. The severity of these reactions depends on your individual lactose tolerance, how much lactose you consumed, and other factors that might affect your gut health.
It’s also important to differentiate between lactose intolerance and a milk allergy. A milk allergy involves your immune system reacting to milk proteins, and even small amounts can trigger significant reactions shortly after consumption. Unlike lactose intolerance, allergic reactions often affect the entire body and can include symptoms like swelling, hives, and shortness of breath.
To stay on top of things, maintain a food and symptom journal. Record what kind of dairy you consumed, when you ate it, and any reactions you experienced. Include digestive symptoms like bloating, gas, diarrhea, or cramps, as well as other unusual reactions. Pay attention to delayed or cumulative symptoms that may worsen over time, and note any changes in energy or mood to identify patterns. For some, symptoms may intensify with repeated exposure, even if the first serving seemed manageable.
When to Contact Your Doctor
If your symptoms become more intense or don’t go away, it’s time to consult a doctor.
Seek immediate medical help if you notice signs of anaphylaxis, such as difficulty breathing, widespread hives, severe swelling, or a sudden drop in blood pressure. Anaphylaxis is a life-threatening emergency that requires urgent care.
If severe symptoms persist after 2–3 weeks of avoiding dairy, it’s a good idea to reach out to your doctor. For those with a confirmed milk allergy and detectable IgE antibodies, reintroducing dairy should only happen under medical supervision, especially if your initial reactions were severe.
Children and individuals with known or suspected allergies should only attempt elimination diets with medical guidance. If you plan to eliminate multiple food groups or have a history of severe reactions, consult a doctor or dietitian before starting the process.
If symptoms resurface during the reintroduction phase, even after successfully completing the elimination period, experts recommend extending the elimination diet for another 3–6 months before trying again. This additional time can give your digestive system more opportunity to recover, potentially improving your tolerance.
Lastly, if there’s any uncertainty about whether milk caused a severe reaction, an oral food challenge may not be advisable, especially for those with a history of anaphylaxis. Your safety should always take priority during the reintroduction process.
How milktab Can Support Your Dairy Reintroduction
If your elimination diet confirms lactose intolerance, dairy doesn’t have to be off the table. Lactase enzyme supplements like milktab can make reintroducing dairy more manageable. As you work through the milk ladder, enzyme support can ease discomfort and help you test your tolerance effectively. Here’s why milktab stands out.
What milktab Offers
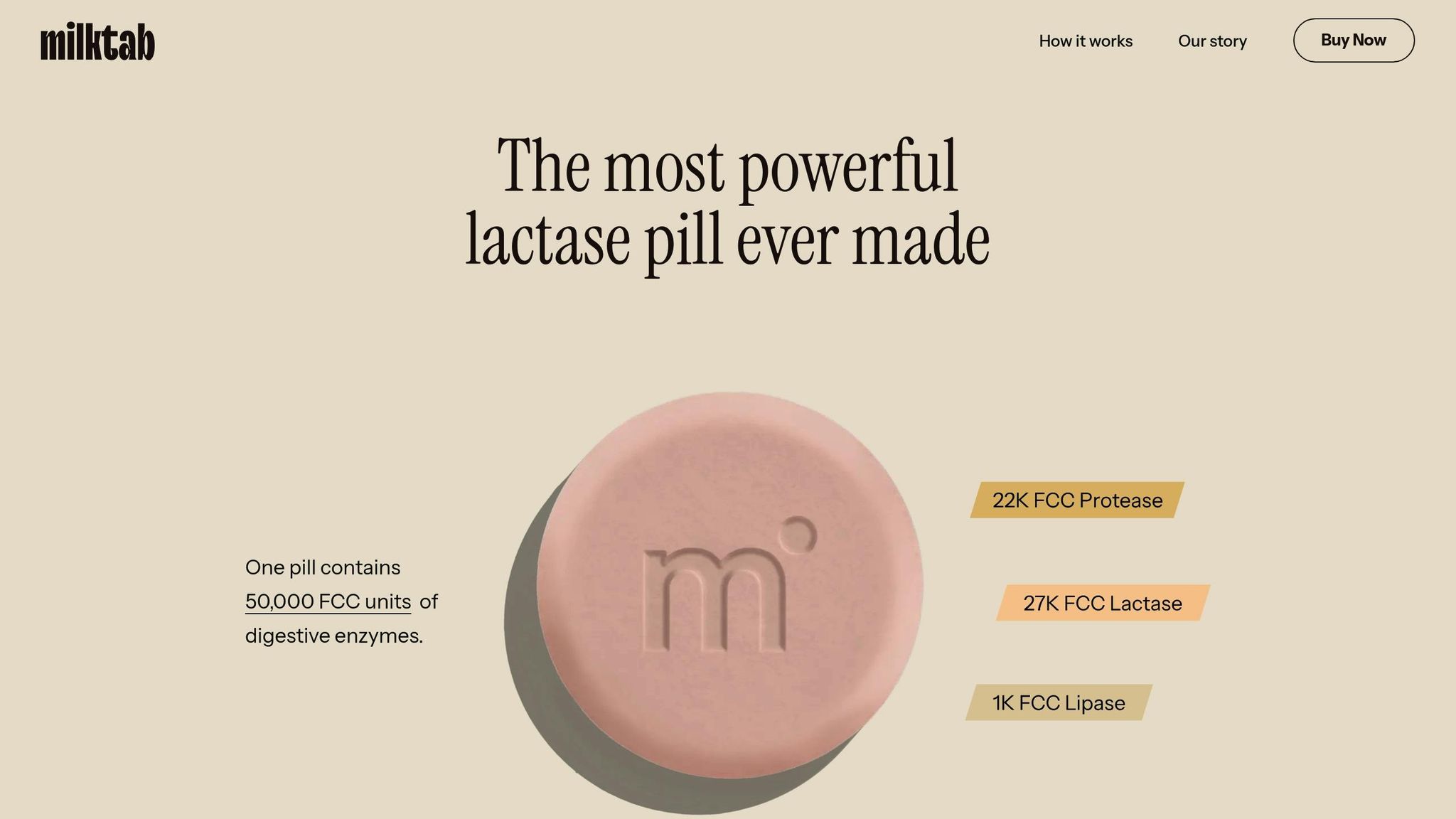
milktab is designed with a triple-enzyme formula that targets lactose, protein, and fat digestion. Each pill packs 27,000 FCC units of lactase to break down milk sugars, 22,000 FCC units of protease to digest milk proteins like casein, and 1,000 FCC units of lipase to handle milk fats. This comprehensive mix tackles multiple elements of dairy that can cause digestive trouble.
"With 27,000 FCC units of lactase, milktab is the strongest lactase supplement on the market." - milktab
These pills are vegan, non-GMO, FODMAP-free, and undergo third-party testing. Their compact packaging makes them easy to carry, so you’re always prepared.
Users frequently highlight milktab’s effectiveness in reducing dairy-related discomfort, allowing them to enjoy a range of products, from milk to ice cream. To get the best results, take milktab with your first bite or sip of any dairy product. This ensures the enzymes are ready to work as soon as lactose enters your system, minimizing symptoms.
Advantages of Using Enzyme Supplements
Incorporating milktab into your dairy reintroduction process offers several benefits compared to going without enzyme support:
| Aspect | With milktab | Without Enzyme Support |
|---|---|---|
| Symptom Management | Reduced bloating, gas, and discomfort | Full-blown lactose intolerance symptoms |
| Dietary Flexibility | Enjoy higher-lactose foods like milk and ice cream sooner | Limited to very low-lactose options for longer |
| Confidence Level | More confidence trying new dairy products | Worry about severe reactions |
| Social Situations | Participate in meals with dairy | Avoid or limit social eating situations |
| Reintroduction Speed | Progress through the dairy ladder more quickly | Slower, more cautious progression |
These benefits make the reintroduction process smoother and less stressful. However, it’s important to note that lactase supplements like milktab are an addition to dietary management, not a replacement. They help bridge the gap while you figure out your personal tolerance levels.
milktab has earned a 4.3/5 star rating on Amazon, based on 67 global reviews. Customers frequently praise its effectiveness and portability. Plus, volume discounts (10% off for 2 boxes and 20% off for 3 boxes) make it a practical choice for anyone looking to manage symptoms while enjoying dairy again.
Key Points for Successful Dairy Reintroduction
To ensure a smooth and safe reintroduction of dairy into your diet, here are some important steps to follow:
Take it slow and start small. Begin with low-lactose options in tiny amounts. This gradual approach allows you to gauge your personal lactose tolerance. Many people with lactose intolerance can handle small portions without experiencing symptoms.
Keep track of your symptoms. Use your symptom log to monitor any reactions. Symptoms may show up quickly or take up to 72 hours to appear. Watch for serious signs like rash, swelling, vomiting, breathing issues, or dizziness - if these occur, stop immediately.
Follow the milk ladder gradually. Refer back to the milk ladder discussed earlier and move through the stages one at a time. If you experience a reaction, step back to the last stage you tolerated instead of giving up entirely. Some people who react to fresh milk may find they can handle milk in cooked or baked forms.
Consider enzyme support. Using lactase enzyme supplements, such as milktab, can help make the process easier. These enzymes break down lactose, potentially reducing symptoms and making the reintroduction more comfortable.
Consult a healthcare professional. If reactions persist or you have a history of severe allergies, seek advice from your doctor or dietitian before continuing. As highlighted by the North West Allergy Network:
"Cow's milk reintroduction should only be performed after obtaining advice from your doctor or dietitian".
Give your body time to adjust. Studies suggest that consuming 8 ounces or less of milk with a meal is often manageable for those with lactose intolerance. However, since about 65% of adults worldwide have difficulty digesting lactose, reintroduction may take weeks or even months. While most children outgrow milk allergies, adult tolerance levels can vary greatly.
The goal is to understand your unique tolerance to dairy and build confidence in managing it. Whether you find you can fully enjoy dairy, need to limit it, or rely on enzyme support, this careful process will help you make informed decisions about incorporating dairy into your diet.
FAQs
What symptoms mean I should stop reintroducing dairy and contact a doctor?
If you notice severe symptoms when reintroducing dairy - such as sharp stomach pain, persistent diarrhea, vomiting, or blood in your stool - stop immediately and reach out to a doctor. Similarly, if you experience signs of an allergic reaction, like swelling, hives, or trouble breathing, seek emergency medical care right away.
These issues might point to something more serious than lactose intolerance, making it crucial to get professional guidance for your health and safety.
How do I use a symptom log to track my reactions when reintroducing dairy?
To make the most of a symptom log when reintroducing dairy, jot down any reactions such as bloating, stomach pain, nausea, or diarrhea that occur after eating dairy. Be specific - note the type and quantity of dairy consumed, the time you had it, and how quickly the symptoms showed up.
Keeping this log for several days allows you to identify patterns, pinpoint possible triggers, and track whether your tolerance improves as you slowly increase dairy intake. This approach helps you make thoughtful choices about your diet while reintroducing dairy in a controlled way.
Why should I start with low-lactose dairy when reintroducing it after an elimination diet?
If you're looking to reintroduce dairy into your diet, starting with low-lactose options is a smart way to ease in. This method helps you gauge your body's tolerance without triggering uncomfortable symptoms like bloating, gas, or stomach pain. It's a gradual process that allows your digestive system to adjust.
Low-lactose choices, such as hard cheeses or lactose-free milk, are easier to digest and offer a gentler way to enjoy dairy again. By beginning with smaller portions and paying attention to how your body reacts, you can decide how much dairy fits comfortably into your routine.



